Hepatocellular carcinoma (HCC) is the most common form of primary liver cancer. This form of cancer is most common in people with chronic liver disease, such as hepatitis B or hepatitis C cirrhosis or steatohepatitis, which are major risk factors for developing hepatocellular carcinoma.
To diagnose hepatocellular carcinoma, as a rule, doctors prescribe:
- biochemical tests (blood tests), in particular, the determination of the level of serum alpha-fetoprotein, as well as to assess liver function;
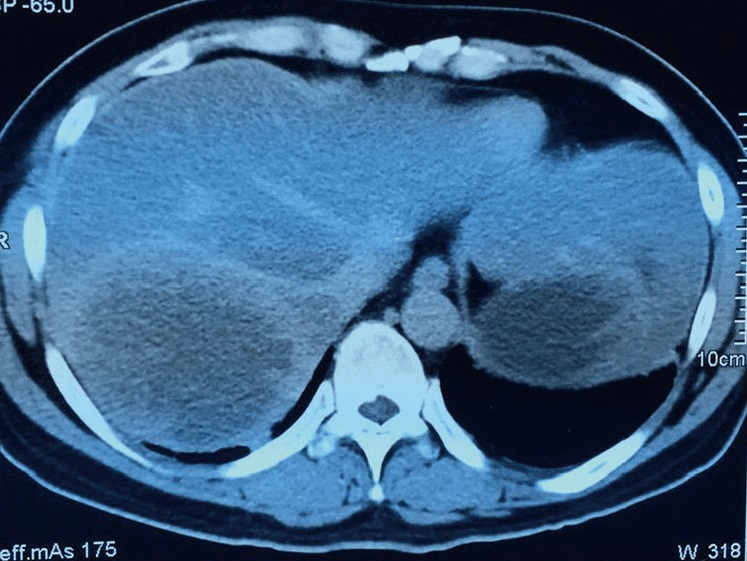
- visual diagnostics (ultrasound, CT and MRI, PET);
- liver biopsy (taking a sample of liver tissue for examination for the presence of malignant cells).
Treatment of hepatocellular carcinoma
Where is the best hospital to treat liver cancer?
Today, there are many options for dealing with liver cancer, and it is natural that most of them will be available when contacting a well-known foreign clinic, such as Medipol University Hospital (Turkey), Anadolu Medical Center or Sourasky Medical Center (Israel).
- Target therapy. Targeted drugs target specific vulnerabilities in cancer cells and help slow the progression of the disease, even in people with advanced liver cancer.
- Immunotherapy. Immunotherapeutic drugs (monoclonal antibodies) use the reserves of a person’s immunity so that he can more effectively attack cancer cells (similar to microbes or viruses). Immunotherapy may be an option for advanced liver cancer.
- Surgery. An operation is performed to remove the tumor and part of the healthy tissue that surrounds it. Surgery may be an option for people with early-stage liver cancer who have normal liver function.
- Liver transplantation. Liver replacement surgery with a donor liver may be an alternative in healthy people whose cancer has not metastasized (it has not spread outside the liver).
- Microwave ablation, cryoablation, and radiofrequency ablation are methods of killing malignant cells using extreme heat or cold. These procedures, also known as cryosurgery or radiofrequency, are usually recommended when surgery is not possible.
- Radiation therapy (radiotherapy) is also recommended mainly when surgery is not possible. A specialized type of radiation therapy, Stereotactic Body Radiation Therapy (SBRT), allows multiple beams to be focused at the same time on a single target point in the body.
- Local radio- and chemotherapy (radio- and chemoembolization) – delivery of chemotherapeutic drugs or radiation (for example, beta particles) directly to the tumor. Using a catheter that conducts radiation or chemotherapy agents through the blood vessels to the liver, drugs can be targeted to the tumor. Radioembolization is also known as SIRT (selective internal radiotherapy).
- Clinical research. Enrollment in a clinical research program provides a chance to try new treatments for liver cancer, although of course there are no guarantees.
Any method of treating hepatocellular carcinoma, as well as any of the drugs indicated for this diagnosis, is selected individually. The treatment regimen for liver cancer may be revised, depending on the results obtained.
Prognosis for hepatocellular carcinoma
In terms of treatment outcomes, the prognosis for hepatocellular carcinoma varies depending on the stage and treatment.
Overall, liver cancer is the fifth most common cancer and the third leading cause of cancer death worldwide. At the same time, there is a more pleasant trend: over the past few decades, the detection of this tumor has changed significantly – thanks to an increase in the level of medical care and routine screenings, hepatocellular carcinoma began to be diagnosed at an early stage, when signs of severe (decompensated) liver disease had not yet appeared. Of course, early diagnosis and promptly started treatment leaves a person with more chances.
However, if we consider this indicator by stages, then the relative 5-year survival rate is:
- 32.6% in patients with localized tumor;
- 10.8% with a disease that has spread beyond the liver, including to the lymph nodes;
- 2.4% with metastatic hepatocellular carcinoma.
In addition, the prognosis largely depends on the degree of liver cirrhosis: the higher the stage, the worse the prognosis, in particular because of the more limited therapeutic options. According to statistics, with hepatocellular carcinoma complicated by cirrhosis, as many patients die from liver failure as from a progressive tumor.
The impact of comorbid conditions (diabetes mellitus, obesity, and other metabolic disorders) on the prognosis of hepatocellular carcinoma continues to be evaluated in studies.
Do you have any questions?
Do you have any questions?
Get a free consultation from our experts