-
 News
A real breakthrough in melanoma treatment: a personalized mRNA vaccine trial
News
A real breakthrough in melanoma treatment: a personalized mRNA vaccine trial
-
 Medical articles
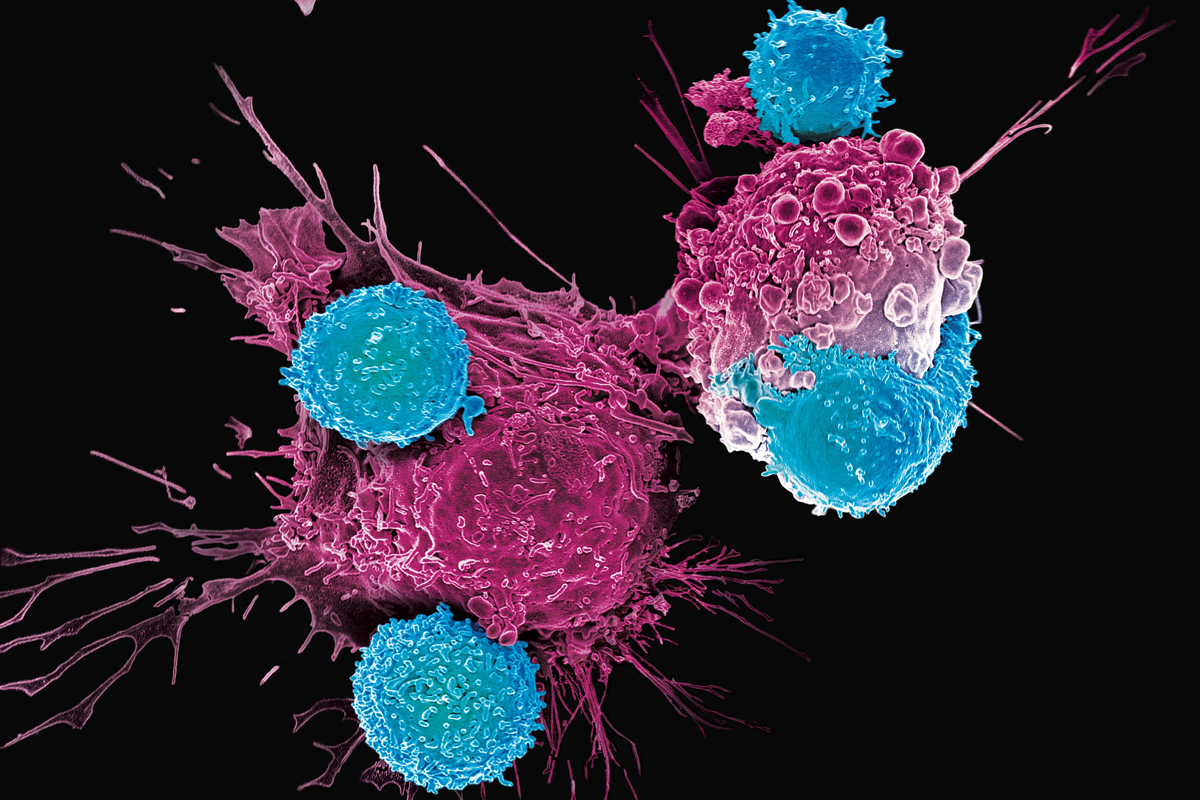
CAR T therapy: helps treat cancer when other methods fail
Medical articles
CAR T therapy: helps treat cancer when other methods fail
-
 Medical articles
Cancer incidence is steadily increasing: disappointing WHO forecast for 2050
Medical articles
Cancer incidence is steadily increasing: disappointing WHO forecast for 2050
-
 Medical articles
Stem cells bring hope to millions of people suffering from hearing loss
Medical articles
Stem cells bring hope to millions of people suffering from hearing loss
-
 Medical articles
TOP 10 clinics for oncology treatment 2023
Medical articles
TOP 10 clinics for oncology treatment 2023
All news
Metachromatic leukodystrophy treatment
Metachromatic leukodystrophy (MLD) — an inherited disorder that causes a wide range of neurological symptoms and ultimately leads to premature death.
The incidence is 1-2 people per 100,000,
- MLD affects people of all ages,
- More often MLD is detected in children under 2.5 years of age, less often in adults.
Diagnosis is made by laboratory tests of urine, blood, and cerebrospinal fluid, as well as imaging (MRI, ENMG) and DNA testing.
Metachromatic leukodystrophy is an incurable, fatal disease.
Treatment for MLD focuses on relieving symptoms.
MedTour patients recommend clinics for the treatment of metachromatic leukodystrophy:
Doctors for the treatment of metachromatic leukodystrophy
Frequently Asked Questions
Metachromatic leukodystrophy (MLD) — a hereditary, constantly progressive pathology that leads to serious damage to the nervous system.
MLD belongs to a group of inherited metabolic disorders. Namely, to lysosomal storage diseases.
MLD is caused by a mutation in the ARSA gene on chromosome 22. Due to a genetic defect, the enzyme «Arylsulfatase A» (ARSA) isn`t produced.
In rare cases, the disease can develop due to a mutation in the PSAP gene on chromosome 10.
MLD is inherited in an autosomal recessive manner: both parents are healthy, but are carriers of the altered gene. The chance that a child will inherit a mutated gene is 25%.
In every human cell, except red blood cells, there are lysosomes. These are cellular structures, the main function of which is the cleavage of various substances with the help of special proteins — enzymes.
Lipid «Cerebroside sulfate» — the most important part of the cell membrane of the nerves (myelin). The breakdown of cerebroside sulfate occurs in lysosomes using the enzyme «Arylsulfatase A». When this lipid is cleaved, building blocks are formed that leave the lysosomes and are involved in the formation of new nerve sheaths.
With a deficiency or absence of the enzyme «Arylsulfatase A», cerebroside sulfate isn`t cleaved, doesn`t leave the lysosome and accumulates in cells. As a result, there is a progressive loss of myelin, which cannot be re-formed. This, in turn, causes various neurological symptoms.
Sulfatide accumulates in the cells of the nervous system, kidneys, gallbladder and liver.
MLD is divided into forms, depending on the age at which symptoms appear and how quickly the disease progresses.
There are three forms:
- Infantile (60%) — up to 2.5 years,
- Juvenile, or adolescent (20-30%) — from 2.5 to 16 years,
- Adult (10-20%) — beginning after 16 years.
Each form progresses with an increase in movement disorders, loss of skills related to learning and behavior.
Infantile form: often children under 1-2 years of age develop normally and do not show any signs of illness. Early symptoms:
- Children start walking later than their peers. It becomes difficult for them to stand and walk if they have already learned this,
- Muscle weakness (hypotonia), sometimes increased muscle tension. Children often stumble and fall (spasticity),
- Impaired coordination.
After a few months, due to muscle weakness, the child is unable to stand and balance.
After a couple of years, the acquired skills are lost. Epileptic seizures, hearing impairment, blindness are observed. Children complain of severe pain.
Juvenile form:
- Early: onset of the disease at 4-6 years of age.
- Symptoms: violation of gait, movement, muscle spasticity, coordination problems. Epileptic seizures join.
- Late: the disease manifests itself at 6-16 years of age.
- Manifestations: Loss of motor function is observed, preceded by learning difficulties and behavioral disturbances.
Adult form: develops after 16 years.
- Symptoms: Mental and behavioral disturbances in the form of mood swings, personality changes and strange behaviors that cause difficulties at work or school. After some time — a regression of mental abilities and the development of dementia. Then movement disorders appear: spasticity, loss of coordination.
Over time, involuntary twisting movements, paralysis, epilepsy, hearing and vision problems, inability to control urination and defecation, as well as loss of speech and perception of the environment join.
The course and severity of the disease, as well as life expectancy, depend on the age at which symptoms appear. Metachromatic leukodystrophy is characterized by continuous progression, high levels of disability and mortality.
Earlier the disease manifests itself, the faster it progresses. Conversely, the later MLD begins, the slower it develops.
- Children with an infantile form now live up to 5-10 years. Most die within 5 years of the first symptoms.
- The life expectancy of patients with a juvenile form reaches 20 years or more. Rarely do adolescents reach adulthood.
- In the adult form, paralysis develops over several years and many patients live for several decades.
Modern methods of diagnosis and treatment of metachromatic leukodystrophy abroad
Diagnostics of the metachromatic leukodystrophy
It’s not difficult for an experienced doctor to diagnose MLD. Based on the available progressive neurological symptoms, the doctor will prescribe the following studies:
- Laboratory tests:
- Blood — used to determine the content and activity of the enzyme arylsulfatase A,
- Urine — to detect the accumulation of cerebroside sulfate,
MRI of the brain: visualizes changes in the white matter of the brain (loss of myelin),
- Spinal cord puncture: cerebrospinal fluid is obtained to detect protein levels and arylsulfatase A deficiency.
- Electroneuromyography: the doctor checks and evaluates the conduction of nerve impulses in response to nerve stimulation,
- Molecular Genetic DNA Testing:
- Prenatal testing (during pregnancy),
- Preimplantation genetic testing for MLD.
Metachromatic leukodystrophy treatment
It’s important to diagnose MLD as early as possible in order to start therapy immediately.
Treatment is aimed at relieving symptoms and compensating for disability.
Symptomatic therapy:
- Epileptic seizures are treated with medication,
- Depression or anxiety is treated with sedatives or antidepressants.
- With severe spasticity, the doctor prescribes muscle relaxants.
Dysphagia and nutritionists can help children who have difficulty sucking and swallowing food or liquids.
Habilitation
Habilitation is support and treatment for people with congenital or early disabilities. The habilitation team has knowledge of how to prevent and reduce the difficulties in daily life caused by disability.
Parents of a child with MLD receive recommendations on how to adapt the child to the home and environmental conditions.
Palliative care
Children with an infantile form live for several years and die early. Palliative care provides painless last months of a child’s life.
Published:
Updated:


Information on this webpage verified by the medical expert




