Calls for Ukraine
Calls for Europe
Calls for USA

The MedTour platform aims to provide patients with access to the most advanced treatment methods. The development of antitumor vaccines is currently one of the most promising areas in oncology. Significant progress has already been made in cancer immunotherapy and a major breakthrough in this field is expected in 2025.
In this article, we will explain what cancer vaccines are, how they work, how effective they are, and also discuss the current state of cancer vaccination in Ukraine.

At the end of the 19th century, New York surgeon William Bradley Coley made an unusual discovery. One of his patients, who was on the brink of death due to a tumor in his neck, unexpectedly recovered after suffering from a severe bacterial skin infection. Intrigued by this phenomenon, Coley decided to replicate the effect by injecting his patients with a mixture of killed bacteria to induce tumor regression. This approach was successful – Coley managed to cure more than a thousand people.
Coley suggested that the infection might activate the immune system, prompting it to fight cancer. However, in his time this hypothesis did not receive proper recognition and was rejected by the scientific community. It was not until the 1950s that researchers began to take notice of Coley’s ideas. Today, his concept is inspiring the development of a new generation of cancer treatment methods known as cancer vaccines. These technologies train the immune system to identify cancer cells and suppress their growth and spread.
Numerous vaccines are currently undergoing clinical trials for the treatment of a wide variety of cancers. After decades of failures and disappointments, scientists have finally achieved encouraging results and 2025 is likely to be a breakthrough year in the field of cancer immunotherapy.
Malignant neoplasms can develop from almost any cell in the body. Normally, the immune system prevents them from spreading by recognizing abnormal cells. T-lymphocytes play a crucial role in this process, as they are able to attack tumors by identifying foreign proteins, called neoantigens, on their surfaces. Natural killer cells and macrophages are also able to find and destroy cancer cells by identifying unfamiliar molecules on their surface or by reacting to antibodies that tag the cells.
However, the peculiarity of cancer cells is their unique ability to develop mechanisms that allow them to become “invisible” to the immune system. This mechanism enables tumor cells to grow, divide and spread throughout the body without interference. Nevertheless, this immune bypass mechanism has opened up new pathways for oncologists to develop medications. Since scientists began sequencing tumor DNA in 2008, they have discovered that cancer cells carry hundreds, sometimes thousands, of mutations that distinguish them from healthy tissue. Some of these mutations lead to the synthesis of abnormal proteins – neoantigens – that can activate the immune system.
The concept of cancer vaccines is based on the introduction of such neoantigens into the body. This approach “teaches” the immune system” to recognize tumors containing these proteins as foreign objects that must be destroyed.

The term “cancer vaccine” can sometimes confuse patients. Many people assume that such vaccines are used exclusively to prevent the development of malignant tumors. However, in reality, the situation is somewhat different. Vaccines of this type are also called therapeutic because they help treat cancer and prevent its recurrence.
Once introduced into the body, vaccine components activate all types of effector lymphocytes, involved in anti-cancer reactions. These include natural killer cells, cytotoxic lymphocytes, antibody-dependent cellular cytotoxicity effectors, and macrophages. In this way, vaccination stimulates the patient’s own immune system to fight the malignant process.
At the same time, preventive cancer vaccines are also being actively researched. Cancer Research UK (CRUK) recently announced funding for researchers from the University of Oxford, the Francis Crick Institute, and University College London to develop a preventative lung cancer vaccine.
This would be the first vaccine designed to prevent lung cancer in a group of patients at high risk of developing the disease. This group includes current or former smokers aged 55-74 years. The new vaccine, known as LungVax, is based on the same technology used in AstraZeneca’s COVID-19 vaccine. Currently, it is in the development phase.
On the other hand, Ukrainian-made xenogenic cancer vaccine CANCERAX (we will discuss it in more detail in the next section) is already actively used to prevent various types of cancer in high-risk patients.
Immuno-oncology is one of the most rapidly developing fields of medicine, focusing on the study of various types of vaccines. These include medications created on the basis of the patient’s autologous immune cells that express tumor antigens, as well as recombinant viral vaccines, peptide vaccines, and DNA vaccines. Below we will review the most promising options.
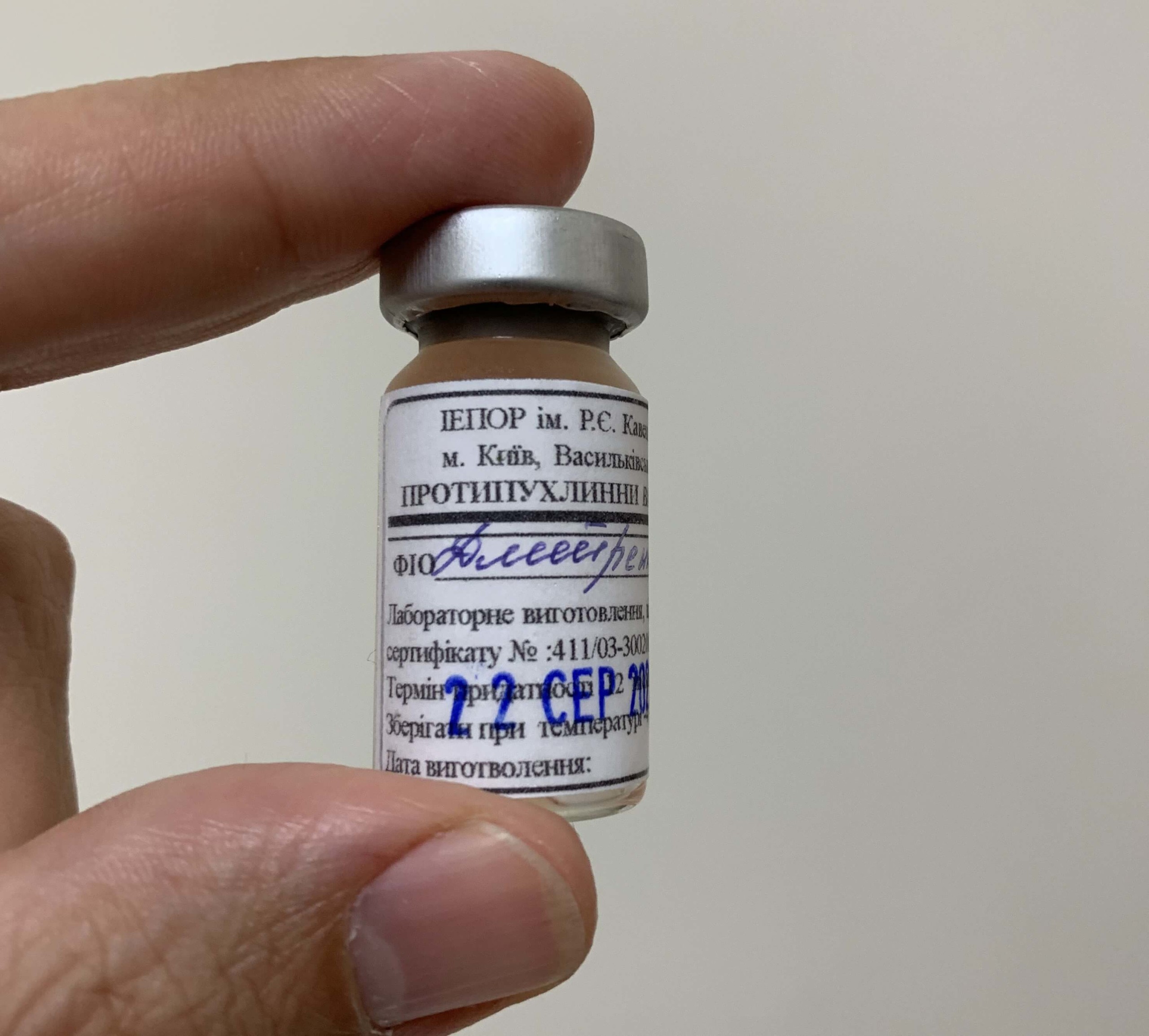
Currently, patients have access to at least two types of antitumor vaccines developed in Ukraine. The autologous vaccine CANCERAX is made from a tumor sample collected after surgery to remove the malignant growth.
Treatment with this vaccine is aimed at preventing the development of relapse and metastases. The medicine contains tumor-associated antigens isolated from a tumor tissue sample. To increase the cytotoxic effect, the antigens are additionally biotransformed under the influence of Bacillus subtilis B-7025 lectin. The goal of therapy is to overcome the tolerance of the immune system to tumor antigens and to form a stable immune response in the patient to the developing malignant process. The CANCERAX autovaccine has proven its effectiveness in the treatment of gastrointestinal tumors, breast cancer, lung cancer, bladder cancer, ovarian cancer, brain cancer, soft tissue tumors, and other types of cancer.
Patients who had surgery a long time ago or do not have a tumor sample can undergo treatment with the CANCERAX xenovaccine. This vaccine contains quail tumor-associated antigens of embryonic origin. These antigens are structurally very similar to human tumor proteins, which lymphocytes can recognize. Administering the xenogeneic vaccine allows the immune system to be “taught” to identify and destroy tumor cells. The xenogenic vaccine CANCERAX helps to stabilize or reduce the activity of the malignant process by 70%.
If you would like to learn more about immunotherapy with cancer vaccines, please contact us. The MedTour coordinating doctor will answer all your questions and offer the best treatment options.

The American company Diakonos Oncology has announced the development of a cancer vaccine that can give hope to patients with an aggressive form of brain tumor – glioblastoma.
The FDA has granted orphan drug status to the dendritic cell vaccine DOC1021, developed by Diakonos Oncology. This opens the possibility of its use for the treatment of newly diagnosed or refractory glioblastoma multiforme in clinical trials in the United States.
DOC1021 medicine is produced using the patient’s dendritic cells and a sample of their tumor, ensuring complete compatibility with the antigen profile of the malignant growth.
The company has already completed recruitment of participants for the Phase 1 clinical trial. The primary goal of this phase is to assess the safety of DOC1021 in patients with glioblastoma who have previously received standard chemotherapy and radiation therapy.
Preliminary results demonstrate a high safety profile for the DOC1021 vaccine with no significant side effects, highlighting its potential in treating one of the most challenging types of cancer.

mRNA vaccines are an innovative treatment method based on the delivery of synthetic mRNA encoding tumor-specific antigens into the body’s cells. These cells then produce antigens that activate the immune system to recognize and destroy cancer cells that express such proteins.
mRNA vaccines target neoantigens – unique mutations that occur exclusively in tumor cells. This allows for the induction of a highly specific immune response. One example of such technology is the mRNA-4157/V940 vaccine developed by Moderna and Merck.
This personalized vaccine is capable of encoding up to 34 neoantigens tailored to the individual tumor profile of each patient. In combination with the immunotherapy drug pembrolizumab (Keytruda), mRNA-4157/V940 showed promising results in a Phase 2b clinical trial in patients with melanoma, significantly reducing the risk of disease recurrence. In October 2024, the developers began Phase 3 clinical trials to confirm the vaccine’s efficacy and safety. If the vaccine is approved for medical use, it is expected to cost about $100,000 per dose.

Pancreatic cancer remains one of the most aggressive and deadly forms of cancer, especially ductal adenocarcinoma. Up to 88% of patients with this diagnosis do not survive, and in 90% of cases the disease relapses within 7–9 months after surgical treatment. However, personalized mRNA-based gene therapy offers a new hope.
A team of researchers from Memorial Sloan-Kettering Cancer Center in New York, in collaboration with the German company BioNTech, has published the results of a small clinical trial involving 16 patients with pancreatic cancer.
The researchers used personalized anti-tumor vaccines to stimulate the immune systems of patients. The scientists extracted tumor tissue from the volunteers and sent it to the BioNTech laboratory in Germany. There, a genetic analysis of mutated proteins on the surface of cancer cells was carried out. Based on the data obtained, specialists created personalized vaccines that take into account the unique characteristics of each patient’s immune system.
As part of the study, participants also underwent chemotherapy and were prescribed a medicine that blocks a protein that helps cancer cells hide from the immune system. The results were encouraging: in half of the patients, the immune system began to recognize and destroy cancer cells. During 18 months of follow-up, no metastases were observed in these patients, demonstrating the potential of this new approach.

French biotech company Transgene has reported promising results from its TG4050 vaccine, developed in collaboration with NEC Corporation. This viral vector-based vaccine is undergoing Phase 1 clinical trials for the treatment of ovarian cancer and HPV-negative head and neck cancer. The results have shown that the vaccine induces a robust immune response in patients, even taking into account the characteristics of weakened immunity in cancer patients.
The ability of the TG4050 vaccine to stimulate immune system activity, including T-cell activation, indicates the high potential of this treatment. Notably, the vaccine has shown efficacy in patients over 65 years of age, as well as in those who initially had low levels of circulating lymphocytes.
The TG4050 vaccine uses neoantigens that are selected individually using the NEC artificial intelligence system, which takes into account the genetic mutations of a specific tumor. This approach offers promising possibilities for treating various types of cancer, enabling personalized therapy tailored to the unique characteristics of the disease in each patient.
Cancer vaccines are becoming an increasingly effective tool in the treatment of various types of cancer. However, their widespread use is limited by their high cost, which is due to several factors.
Additionally, Advanced technologies and specialized equipment involved in the development and production of these drugs also contribute to their high price.
In Ukraine, treatment using antitumor vaccines is more accessible, while the quality of the medicines used is fully consistent with that in the USA, Europe, Israel, and Japan.
MedTour cooperates with leading clinics worldwide that use innovative immunotherapy methods. We are ready to help select the optimal treatment plan for each patient, taking into account their individual characteristics and needs.
Please rate the work of MedTour
