Calls for Ukraine
Calls for Europe
Calls for USA
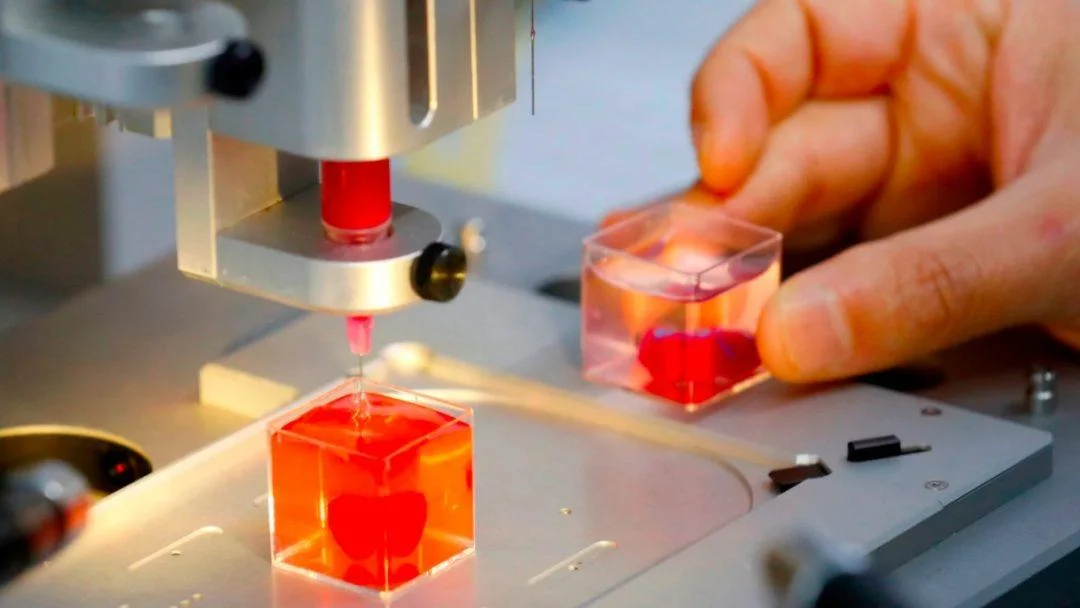
An international team of scientists has just made a major breakthrough in diabetes research by successfully 3D printing functional human islets of Langerhans using new biological ink. One day, this technology could eliminate the need for insulin injections.
As a major breakthrough in diabetes research, a group of scientists led by Dr. Quentin Perrier has developed a method for 3D printing islets — insulin-producing cells found in the tissues of the pancreas.
According to the International Diabetes Federation, islet transplantation is usually performed in the liver, but with limited success, highlighting the need for more effective treatments for the 59 million people worldwide who suffer from type 1 diabetes.
Implantation under the skin is a “major leap forward in diabetes research” that will provide patients with type 1 diabetes with a less invasive and more accessible treatment option. “Our goal was to recreate the natural environment of the pancreas so that the transplanted cells would survive and function better,” explains Dr. Quentin Perrier.
To manufacture pancreatic islets, the team had to precisely adjust the parameters of the 3D printer and use special biological ink that mimics the supporting structure of the pancreas.
The fragility of human islets poses serious problems for medicine. The team of scientists adjusted the printer settings. Low pressure (30 kPa) and low printing speed (20 mm per minute) reduced the physical stress on the islets and helped them retain their natural shape. Previous approaches resulted in the islet structures being destroyed or sticking together.
“Special biological ink made from alginate and decellularized human pancreatic tissue mimics the supporting structure of the pancreas, providing the islets with oxygen and nutrients necessary for their survival,” explained Dr. Perrier.
Laboratory tests showed that the bio-printed islets remained alive and healthy, with a cell survival rate of over 90%. Cells printed with special biological ink remained alive and functional for three weeks, confirming their potential for clinical use. They responded better to glucose than standard islet preparations, secreting more insulin when needed.
By day 21, the islets demonstrated a higher ability to sense and respond to blood sugar levels, suggesting to the scientists that they may have achieved real success. Perhaps the key factor was the porous architecture of the 3D-printed islets, which provided oxygen and nutrient supply and promoted vascularization, which is very important for long-term survival and function after transplantation.
Please rate the work of MedTour
