Calls for Ukraine
Calls for Europe
Calls for USA
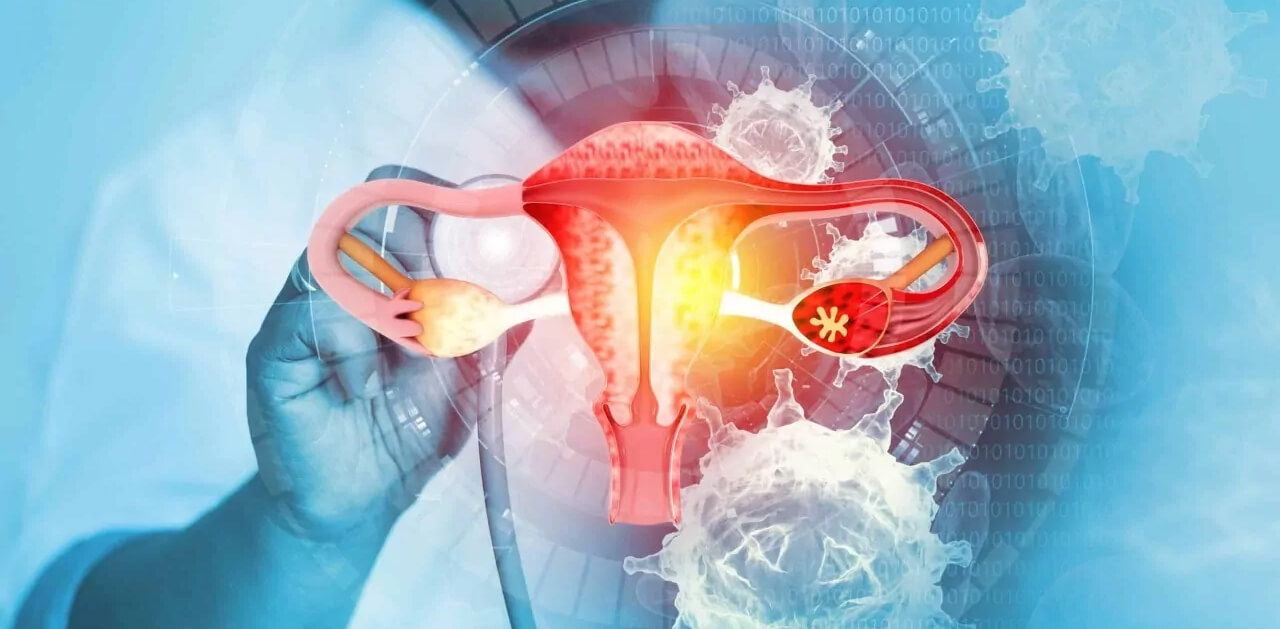
Cervical cancer (CC) is one of the most well-known malignant diseases that occurs in women. According to statistics, this pathology ranks 3rd in cancer incidence among women and is considered one of the main causes of death from malignant diseases. According to statistics, about 300 thousand women die from this pathology every year. However, this number can be significantly reduced with proper prevention.
Cervical cancer can develop quite early and is often diagnosed between 35 and 50 years of age. Moreover, if this disease can be detected in the early stages of development, it responds quite well to treatment. But it is even more effective to prevent the development of this disease, and this can be achieved through prevention. The most important preventive measures include vaccination, as well as regular screening examinations and timely therapy. Proper prevention of cervical cancer makes it possible to significantly reduce the number of women diagnosed with this disease and avoid many deaths associated with it.
MedTour will help you find a clinic where you can undergo all the necessary preventive measures: get a vaccine, undergo an examination, choose the optimal treatment if cervical pathologies are detected.
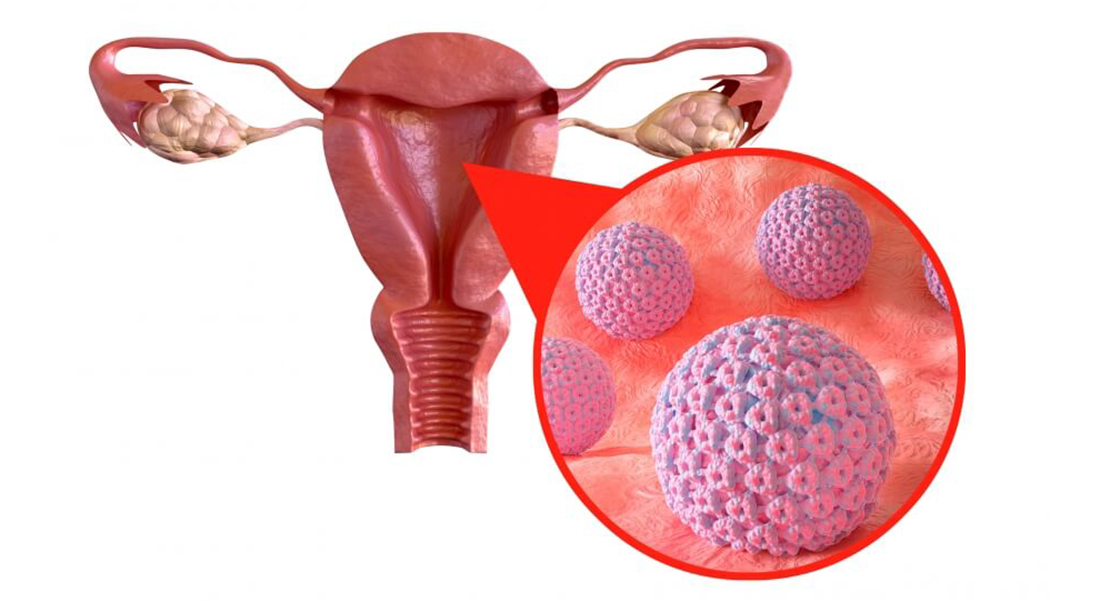
In most cases, cervical cancer is caused by the human papillomavirus (HPV) entering a woman’s body. Papillomavirus is considered the most common sexually transmitted infection. It infects about 80% of people who have an active sex life. There are about 100 types of HPV, but not all of them cause cancer. Currently, 19 HPV strains of high oncogenic risk have been identified. These types can trigger the occurrence of cervical cancer or other oncological pathologies. Moreover, most often (in more than 70% of cases) the development of a malignant neoplasm in the cervix is associated with the entry of HPV serotypes 16 and 18 into the body. Another 5 strains of HPV cause about 20% of malignant diseases of the cervix.
The entry of HPV into the body does not necessarily lead to the appearance of tumors. In approximately 90% of cases, the female body fights the virus on its own and over time the infection completely disappears without causing noticeable harm. But if a woman’s body is weakened, the immune system does not work well enough, and a number of provoking factors are present, then exposure to HPV can lead to precancerous conditions, and over time, to the development of cervical cancer.
In addition to HPV, several factors can contribute to the occurrence of cervical cancer:

In the very first stages of development, cervical cancer often does not produce any specific symptoms. Therefore, it is very important for women to regularly undergo routine preventive examinations. However, there are a number of symptoms that are most characteristic of this malignant disease:
If these signs appear, you need to see a gynecologist as soon as possible and undergo an examination that will determine the causes of these symptoms. If the disease is detected in the early stages and the correct treatment is selected, then the probability of complete recovery is more than 90%. However, it is much easier to avoid the occurrence of a disease than to treat it later. Therefore, today much attention is paid to the prevention of this pathology.
Today, to combat cervical cancer in the world, experts use an integrated approach. And prevention measures play an important role in it. WHO has developed a global strategy to fight cervical cancer. As part of the strategy, a number of preventive measures are proposed, which, according to scientists, will help reduce the incidence of cervical cancer by 42% by 2045 and by 97% by 2120.
There are primary, secondary and tertiary prevention of cervical cancer, and a set of measures and activities has been developed for each stage.
As part of the primary prevention of cervical cancer, sex education is carried out, and awareness-raising work is carried out about the need for barrier contraception and hygiene of sexual relations. But the main measure for the prevention of cervical cancer is timely vaccination against papillomavirus.
Vaccination is recommended for girls before the onset of sexual activity at the age of 9-15 years. But if necessary, it can be carried out later, up to 45 years. Also, in some cases, HPV vaccination may be recommended for boys, since this virus can provoke the development of malignant neoplasms in boys.

Secondary prevention of cervical cancer includes screening examinations and tests aimed at identifying papillomavirus in the body and detecting cancer or precancerous conditions.
According to international standards, screening tests for HPV DNA and HPV mRNA are recommended for the prevention of the disease. These tests will detect dangerous strains of papillomavirus in the body, if they are present. Annual screening is recommended for women between 25 and 50 years of age. Over 50 years old, diagnostics can be done once every 5 years.
If precancerous conditions are discovered during the examination, their timely treatment is necessary. Precancerous conditions that can eventually develop into cervical cancer include dysplasia, leukoplakia with atypia, and erythroplakia. When they appear, it is necessary to undergo treatment as quickly as possible. This is also a prevention of cervical cancer, as it will help prevent its development.
Recently, the term tertiary prevention of cervical cancer has been actively used. In this case, we are talking about women who have already encountered this disease. Tertiary prevention involves treatment of cervical cancer (surgery, radiation therapy, chemotherapy and the use of other methods), as well as measures that allow a woman to return to a full life after treatment. This includes therapeutic measures, physical and social rehabilitation.

Perhaps the most important part of preventing cervical cancer is vaccination. It has been proven that the use of vaccines is an effective prevention of cervical dysplasia and other precancerous conditions. There are currently four WHO-approved vaccines in the world. But in Ukraine and many other countries, two vaccines, Gardasil and Cervarix, have been registered and are actively used. All existing vaccines protect against human papillomavirus strains 16 and 18. But some have a broader spectrum of action and can protect against some other strains of HPV. Cervarix protects against strains 16 and 18, while Gardasil is called a quadrivalent vaccine because it protects against four strains of HPV – 16,18, 6 and 11.
The World Health Organization recommends routine HPV vaccination, and many countries have already included these vaccines in the vaccination schedule.
To achieve the desired effect, it is necessary to do several vaccinations at a certain time interval. The use of such vaccines is safe and provides a high degree of protection. Side effects may include short-term pain and redness at the injection site, and sometimes a slight increase in temperature may occur.
In addition to HPV vaccinations, there are other vaccination options for cervical cancer. Today, cancer vaccines are being actively developed. Their action is aimed at “teaching” the immune system to detect and destroy cancer cells. At the Institute of Experimental Pathology, Oncology and Radiobiology named after. R. E. Kavetsky in Ukraine created a xenovaccine that can be used to prevent various types of cancer. It is produced on the basis of embryonic tumor-associated antigens of animal origin, which are similar to tumor antigens. The introduction of such a vaccine into the body helps the cells of the immune system detect cancer cells and respond more actively to them. A xenovaccine for the prevention of cancer pathologies can be used for people who are at risk, as well as for those who have precancerous conditions. It can also be used to treat cancer in combination with other therapies.
There is another type of cancer vaccine – autovaccines. They can be used as part of tertiary prevention, that is, for those who have already been diagnosed with cervical cancer and had the tumor removed. Autovaccines are made individually from tumor tissues of a person exposed to the disease. Their use allows the body to intensify the immune system’s fight against cancer. Such vaccination is recommended to prevent relapses and to avoid the occurrence of metastases.
The MedTour coordinator will advise you on different types of vaccines and help you choose the best option.
The MedTour platform will help you get to a clinic that offers preventive measures for primary, secondary and tertiary prevention. We will offer you the best medical centers that provide vaccinations, diagnose and find optimal treatment options for precancerous conditions and cervical cancer.
You can get vaccinated against HPV in many clinics around the world. MedTour will help you make the best choice based on your wishes. If you want to use an cancer xenovaccine or an autovaccine, we cooperate with clinics in Ukraine and Turkey that provide such vaccination. The MedTour coordinator will tell you in detail about the options and answer all your questions.
Contact us to find the best doctors who treat and prevent uterine cancer. The MedTour platform cooperates with specialists around the world who have extensive experience and a good reputation. We will help you find a doctor who can offer you the full range of necessary medical services. Call us or send a request to get a free consultation with a MedTour coordinating doctor.
Please rate the work of MedTour
