Calls for Ukraine
Calls for Europe
Calls for USA
For many years, scientists have been trying to find a way to defeat cancer forever or come up with an effective medicine against which this insidious disease would have no chance. One possible solution to this problem is the creation of an anti-cancer vaccine that could prevent the transformation of healthy cells into malignant ones. Unfortunately, so far this method has been discussed only theoretically.
In his book The Role of the Immune System in Cancer Treatment, Marius Strioga, an oncoimmunologist at the Lithuanian National Cancer Institute, writes about how immunity is formed. When various pathogenic microorganisms, such as bacteria or viruses, first enter the body, a specific immune response is formed.
It can take two forms. The short-term effector response involves the work of temporary cells-soldiers of the immune system, which destroy the enemy and die. But there is also the immunological memory response, in which the soldiers of the immune system continue to patrol the body for an extended period of time. This response may last for several years, decades, or even a person’s entire life.
According to Marius Strioga, the purpose of prophylactic vaccination is to create an immune readiness in the body for a specific pathogen and thus protect against the disease caused by it.

When developing prophylactic vaccines against microbes that cause infectious diseases, the choice of antigen is quite unambiguous, since all pathogen molecules are foreign to the human body and are usually easily detected by the immune system. The situation is completely different in the case of cancer.
Cancer cells are abnormally altered but still the body’s own cells, and the immune system is “trained” not to attack its own cells or the molecules they release.
Tumor cells contain altered proteins that tell the immune system that the cell containing them is abnormal. However, changes in these proteins may be too small for the immune system to notice and consider them dangerous to the body. At the same time, cancer cells undergo changes in the structure or expression of various proteins. But it is difficult to predict in advance what they will be and in what proteins they are formed when a normal cell turns into a cancer one. Therefore, finding an antigen for a prophylactic cancer vaccine is very difficult.
Theoretically, the situation is not hopeless if you look at the so-called universal cancer antigens, that is, proteins (eg, such as telomerase, survivin). Without them, malignant cells cannot exist. These antigens are found in cells of almost all forms of cancer.

Universal cancer antigens appear to be ideal targets for the development of preventive cancer vaccines. But there are some nuances that must be taken into account. For example, certain universal antigens are also present in some normal cells of the body (for example, in the stem cells of various organs, which are extremely important in maintaining the long-term functioning of these organs).
Therefore, the possibility cannot be ruled out that a long-term protective immune response to universal cancer antigens elicited by a prophylactic vaccine may eventually cause soldiers to recognize and attack normal cells bearing these antigens. Such an autoimmune attack (directed against one’s own cells) can have extremely negative consequences for the body.
According to Marius Strioga, preventive vaccines against cancer should be complex, that is, capable of inducing the formation of both protective antibodies and cytotoxic memory T-lymphocytes.

It is very difficult to develop one preventive vaccine against all types of cancer, because even two tumors of the same type in different people differ from each other.
If different patients have the same form of cancer, they are not the same from an immunological point of view. Moreover, even in the same patient, cancer cells change over time. Therefore, it is unlikely that it will be possible to develop a universal vaccine against all types of cancer.
There are also difficulties in creating vaccines for different types of malignant tumors. Unless it’s cancer associated with a specific mutation. For example, people who inherit BRCA1 or BRCA2 gene mutations have an increased lifetime risk of developing breast cancer, ovarian cancer, and prostate cancer, as well as an increased risk of melanoma, pancreatic cancer, and colon cancer.
It would seem that these inherited mutations could be an excellent target for a prophylactic vaccine against the development of these tumors. However, even in this case, the situation is not as simple as it seems at first glance. In the body, each protein is encoded by two forms of the same gene – alleles, one of which is inherited from the father, and the other from the mother.

Usually, only one mutated allele of the BRCA1/2 gene is inherited, so a person does not get cancer, because in order for it to develop, the second allele must also mutate. At the same time, such people have an increased risk of developing breast, ovarian, or prostate cancer, because they already have one mutant allele and a mutation of the second is enough for the cell to become malignant.
It is important to note that after inheriting one allelic mutation in the BRCA1/2 gene, normal cells also have it. Therefore, by activating the immune response against such a mutation, there is a possibility that the immune system may mistakenly recognize and attack normal cells that have only one mutated allele and are not yet cancerous. Thus, a highly undesirable autoimmune attack on healthy tissue cells is possible.
Vaccines are currently being developed against viruses whose chronic infection can cause cancer. For example, there are vaccines against:
However, the creation of a preventive vaccine against cancer is problematic in itself, because it is impossible to predict when and what mutations will turn a normal cell into a cancer one. But the development of therapeutic antitumor vaccines is underway.

Therapeutic vaccines are used when a person already has a certain disease, such as a chronic infection or cancer. In this case, vaccination is carried out not for prevention, but for therapeutic purposes. That is, this is not an attempt to prevent a threat, but a fight against a real problem that already exists. The goal of a therapeutic vaccine is to “show” or “remind” the immune system what it has to fight against.
In this case, the target already exists, and there is no need to assume what mutations will occur in the cells. The results of various studies and clinical experience show that therapeutic cancer vaccination is particularly effective when properly combined with other cancer treatments.
If a person develops cancer, then the malignant cells in his body have managed to “cheat” the immune system. Thus, therapeutic vaccination for cancer aims to induce a targeted anti-tumor immune response and help the immune system recognize cancer. In other words, the goal is to reprogram a deficient or cancer-balanced anti-tumor immune response and return it to a normal, physiological state that protects the interests of the body (control of cancer cell growth).

Therapeutic cancer vaccination can be used to provide an antitumor immune response that protects the body from cancer recurrence and progression. It can also be used to increase the sensitivity of malignant cells to standard cancer treatments, especially radiotherapy and chemotherapy.
Therapeutic vaccines do not directly attack cancer and do not come into direct contact with the cells that make up the tumor. The purpose of these vaccines is to stimulate the formation of functionally active cytotoxic T-lymphocytes. They are the main soldiers of the immune system, destroying cancer cells. These lymphocytes can only be fully activated by properly matured dendritic cells.
The effect of therapeutic vaccination is based on the ability of properly matured dendritic cells to trigger a targeted immune response that can control the activity of cancer cells in the body.

Marius Strioga believes that therapeutic vaccination is still not a standard treatment for cancer, as there are not enough randomized clinical trials with a large sample. They are not carried out partly because the big pharmaceutical companies are not particularly interested in this treatment method, since such vaccines cannot be mass-produced.
Therapeutic vaccination is prescribed to each patient individually, taking into account the histological form of the malignant disease, its stage, course, previous treatment and response to it, as well as the presence of concomitant diseases.
The dendritic vaccine is produced separately for each patient. It cannot be manufactured in factories on an industrial scale. There are very strict requirements for taking blood from a patient, manufacturing the drug, storing and transporting it, and administering it to the patient. Therefore, in terms of logistics and profitability, this is not an attractive treatment option for pharmaceutical companies.
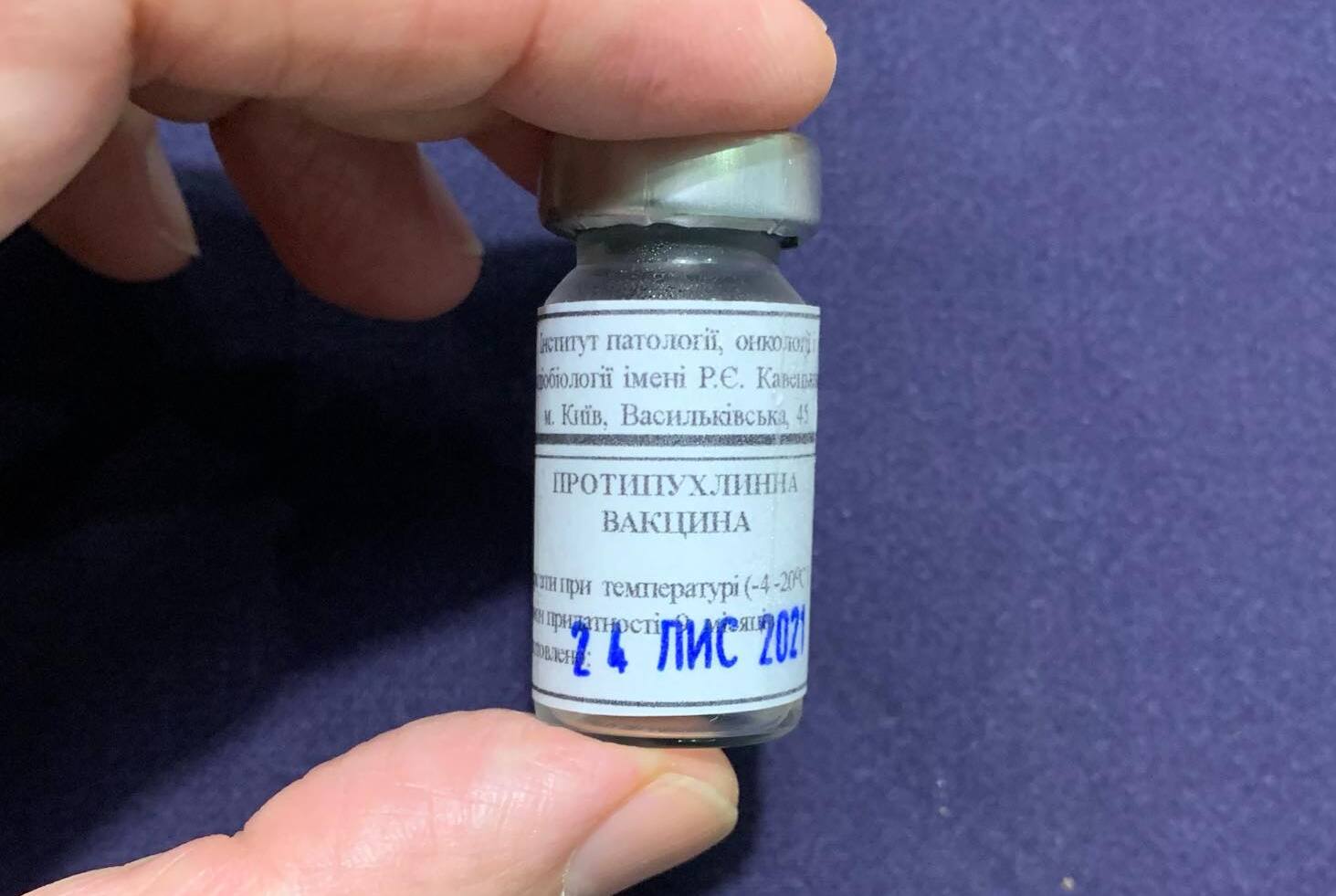
In Ukraine, the direction of immunotherapy with antitumor vaccines is at the stage of active development. The Kavetsky Institute of Pathology, Oncology and Experimental Radiobiology has developed vaccines that improve the immune response and activate the body’s own defenses in the fight against cancer. To create drugs, scientists used proteins obtained from animal material, as well as autologous cells. They were also the first in Ukraine to use the B. subtilis B-7025 cytotoxic lectin to improve the effectiveness of vaccines.
Ukrainian antitumor vaccines are as effective as their counterparts made in the USA, Europe and Japan, but at the same time they have a much lower cost.
MedTour company is actively collaborating with medical centers around the world that offer innovative cancer vaccine therapy. If you are interested in this advanced treatment method, please fill out the online form or call any of the phone numbers listed on the site. Our doctor-coordinator will contact you shortly and hold a free consultation.
According to oncoimmunologists, the clinical response to therapeutic vaccination depends on the form and stage of the malignant disease. Immunotherapy is most effective when combined with standard cancer treatments.
Marius Strioga believes that therapeutic vaccination is best for early cancers, before the tumor has developed mechanisms to escape immune system surveillance. At an early stage of the course of the disease, it is possible to remove malignant foci from the body surgically or with the help of radiation therapy. The goal of therapeutic vaccination is to delay the possible recurrence or progression of the disease as long as possible.
Please rate the work of MedTour
