Calls for Ukraine
Calls for Europe
Calls for USA
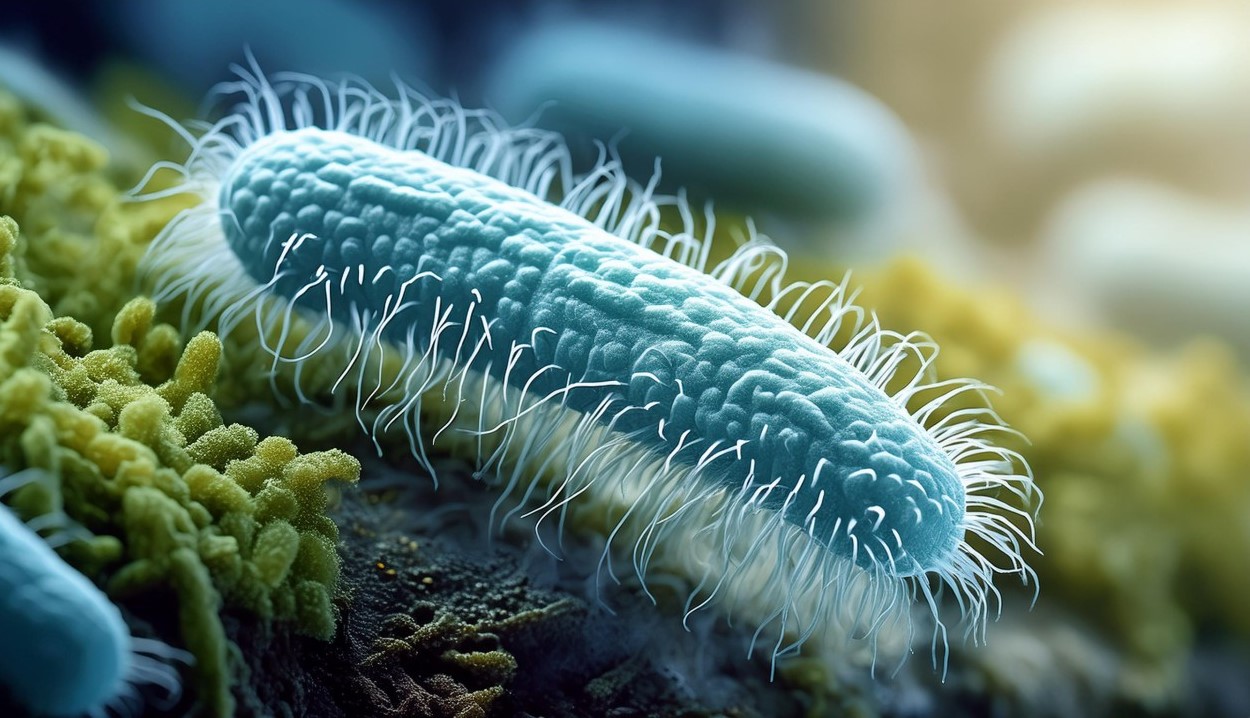
Researchers at Columbia University have created probiotic bacteria that train the immune system to destroy cancer cells. This paves the way for a new class of cancer vaccines that use the natural properties of bacteria to target tumors. Such microbial cancer vaccines could be personalized to target the primary tumor and metastases in a specific individual, and could even prevent future recurrences of the disease.
In studies on mouse models of colorectal cancer and melanoma, the bacterial vaccine boosted the immune system, suppressing the growth of primary and metastatic cancerous tumors and in many cases destroying them. At the same time, it had no effect on healthy parts of the body.
The bacterial vaccine was much more effective than the therapeutic peptide-based cancer vaccines used in numerous previous clinical trials.
“An important advantage of our system is its unique ability to coordinately rewire and activate all parts of the immune system, inducing a productive antitumor immune response. We believe this is why the system works so well in models of solid tumors, which are particularly difficult to target with other immunotherapies,” said Andrew Redenti, a postdoctoral fellow at Columbia University’s College of Physicians and Surgeons who helped lead the study.
Bacterial vaccines can be personalized for each type of tumor. “Every tumor is unique, because tumor cells carry certain genetic mutations that distinguish them from normal healthy cells. By programming bacteria to force the immune system to target these cancer-specific mutations, we may be able to develop more effective therapies that can induce a patient’s own immune system to detect and destroy cancer cells,” said Nicholas Arpaia, PhD, associate professor in the Department of Microbiology and Immunology at Columbia University College of Physicians and Surgeons, who led the study.
Bacteria have been used to treat cancer since the late 19th century when William Coley, a surgeon at New York Hospital, observed tumor regression in some patients who were injected with bacteria into inoperable tumors. The bacteria are still used today as a therapeutic agent to treat patients with early-stage bladder cancer.
Researchers now know that some bacteria can naturally migrate into tumors and colonize them, thriving under conditions of frequent oxygen deprivation and triggering a local immune response. However, when used in this way, the bacteria usually cannot precisely control or direct the immune response to attack the malignancy.
“By themselves, these characteristics do not give the bacteria enough power to stimulate an immune response capable of destroying a tumor, but they are a good starting point for creating a new area of cancer therapy,” the researchers said.
The new system is based on a probiotic strain of E. coli. Scientists have made many genetic modifications to it to precisely control the way the bacteria interact with and train the immune system, and reliably achieve tumor destruction.
Due to the nature of the bacterial system and additional genetic modifications made by scientists, these bacterial cancer treatments also resist the immunosuppression mechanisms that tumors use to counteract the immune system.
As a safety measure, the genetic modifications also block the bacteria’s innate ability to evade immune attacks directed against themselves. This means that engineered bacteria are easily recognized and destroyed by the immune system and are quickly eliminated from the body if they don’t find a tumor.
The first step in creating such microbial vaccines for humans will be determining the sequence of the patient’s cancerous tumor and identifying its unique neoantigens using bioinformatics methods.
When injected into a patient with a tumor, the bacteria would navigate to the neoplasm, settle there, and steadily produce and deliver their payload of “ medication” there. After activation of the bacterial vaccine, the immune system will be forced to destroy the cancer cells that have spread throughout the body and prevent further development of metastases.
Please rate the work of MedTour
