Calls for Ukraine
Calls for Europe
Calls for USA

Testicular cancer is a malignant tumor that affects the male sex glands. 90% of this type of cancer begins in germ cells. Some neoplasms develop outside the testicle. As the malignant process progresses, it can spread to the lymph nodes in the abdominal cavity, liver, intestines, lungs, and brain.
The incidence of testicular cancer is increasing all over the world, however, in Western countries in recent decades, there has been a decrease in the death rate. This is due to the fact that the field of oncology is developing rapidly. There are new diagnostic methods that allow to detect the disease at an early stage. Effective treatments are being developed.
One of the latest innovations in this area is vaccine therapy. The use of cancer vaccines helps to “tune” the immune system so that it can recognize and destroy cancer cells on its own. Cancer vaccines are used as part of complex therapy to increase its effectiveness and reduce the risk of recurrence of the disease. More information about the new method of cancer treatment can be found in the “Treatment” section.
The exact causes of the disease are unknown, but there are factors that increase the risk of developing it. These include:
Having the conditions listed above does not necessarily mean that a person will develop cancer. However, men who are at risk need to be more attentive to their own health and undergo regular oncological examinations.

Common symptoms of the disease are:
Some tumors produce androgens (male sex hormones) or estrogens (female sex hormones). Estrogen-producing neoplasms can provoke a decrease in libido. Androgen-producing tumors are not associated with any specific symptoms in men, but in boys they cause facial and body hair to grow at an abnormally early age.
Germ cell tumors are the most common type of testicular cancer. They are divided into two main types:
Sometimes testicular cancer is mixed, that is, it contains seminoma and non-seminoma cells. In this case, it is treated as if it were nonseminoma cancer.
A small number of testicular tumors begin in the cells that make up the supporting (structural) and hormone-producing tissue of the testicles. They are called stromal. The two main types of stromal tumors are neoplasms arising from Sertoli cells and Leydig cells. They are usually benign and are well treated with surgery. Other types of cancer, such as lymphoma, can also affect the testicles.

At the first stage, the doctor conducts a physical examination and examines the patient’s history. Further, the specialist prescribes laboratory and instrumental studies:
Laboratory tests for tumor markers are also carried out:
The level of tumor markers is necessary to assess the risk of disease recurrence after surgery. The test results help doctors plan further treatment.
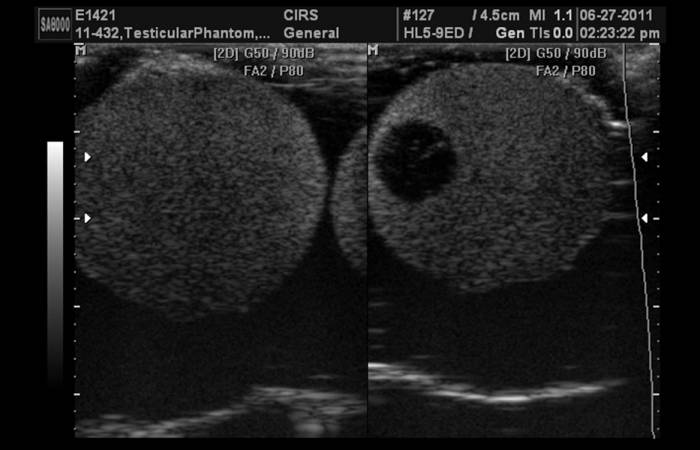
Ultrasound is the main imaging modality for testicular tumors due to its high sensitivity, low cost, and availability of this diagnostic technique. Ultrasound helps to distinguish cancer from a benign tumor.
Due to its low discriminative power, ultrasound is not suitable for tumor staging, so CT is used for this purpose. The final diagnosis is made not on the basis of the results of imaging studies, but after a histological analysis of the removed tumor.
Before starting treatment, a urologist and oncologist should discuss the treatment regimen with the patient. The choice of therapeutic tactics will be based on the stage of cancer, its location, age and personal preferences of the man. Patients should be aware that anticancer therapy may adversely affect their fertility. Therefore, men who wish to have children in the future may freeze their sperm.
Testicular cancer surgery
Surgery is the main method of treatment. The removal of the testicle is called an orchiectomy. Most often, the operation is performed through a small incision in the groin. A tumor sample is sent for histological analysis. According to its results, further treatment is prescribed. For men who are concerned about the appearance of the genitals, a testicular prosthesis is installed.
With spreading cancer, a dissection of the retroperitoneal lymph nodes is performed. This surgery is usually recommended for men with non-seminomas that are prone to recurrence.
Radiotherapy
Radiation therapy is used to kill cancer cells that may have remained after surgery or migrated to the lymph nodes. This treatment is only used for seminomas because some non-seminomas are resistant to radiotherapy. Radiation therapy is also given to patients with brain metastases.
Chemotherapy
It is used for cancer that has spread beyond the testicle or with an increased level of tumor markers after surgery. Chemotherapy drugs are also prescribed to reduce the risk of cancer coming back after surgery.
Cancer vaccines

Vaccine therapy is a new method of treating malignant tumors, the main principle of which is to activate the immune system to fight cancer cells. Currently, there is an active development of antitumor vaccines for the treatment of various cancers. MedTour is committed to making innovative cancer therapies more accessible to its patients. We currently offer treatment with two types of Cancerax vaccine:
Vaccine therapy is an innovative method of anticancer therapy. However, it cannot be perceived as a panacea in the treatment of cancer. Vaccines are used as an adjunct to standard treatment to improve outcomes and reduce the risk of relapse.
To learn more about testicular cancer vaccine therapy, call or fill out the feedback form. Our medical coordinator will answer all your questions in detail and help you organize your treatment.
The prognosis depends on the stage of the disease:
Early detection and timely initiation of qualified therapy are the keys to successful treatment of testicular cancer.
Testicular cancer is highly curable even in patients with metastases at the time of diagnosis. The overall 5-year survival rate is 95.2%. The prognosis varies depending on the histological type of cancer (seminoma or nonseminoma), stage, level of tumor markers, presence and location of metastases. Depending on the stage, the 5-year survival rate is:
With early detection and quality treatment, a patient can live as long as people without cancer.
The MedTour platform cooperates with the world’s leading cancer centers specializing in the treatment of testicular cancer. We will select a clinic that has modern equipment and has access to innovative methods of anticancer therapy. Our coordinators will help resolve all issues related to the organization of treatment. Contact the medical coordinator of MedTour to get a free consultation.
The MedTour platform contains information about leading oncologists who specialize in the treatment of testicular cancer and have been able to achieve significant results in this area. Contact our medical coordinator in any way convenient for you to find the best available specialist for you, taking into account your personal needs and wishes.
Please rate the work of MedTour
