Calls for Ukraine
Calls for Europe
Calls for USA
There are three main signs of cancerous tumors: growth, penetration into surrounding tissues and metastasis to distant areas of the body. The same characteristics can be attributed to sarcomas. However, they are usually called malignant neoplasms, but not cancer.
Cancer arises from the epithelial cells that line most of the cavities and spaces of the human body. At the same time, sarcomas are formed from mesenchymal cells. In the human body, these cells form fat, cartilage, connective tissue, muscle, bone tissue, as well as blood, lymphatic vessels and nerve sheaths.
Distinctive characteristics of sarcomas:
Primary lung sarcomas are a group of nonepithelial malignant tumors developing from mesenchymal lung tissue. They are very rare, accounting for only 1.1% of all malignant lung diseases.

Some of the factors that may play a role in the development of lung sarcomas are the following:
Some researchers believe that chronic bronchitis also plays a role in the development of lung sarcomas.
The danger of malignant tumors lies in the fact that at an early stage they do not manifest themselves in any way. As the tumor progresses, patients experience symptoms such as:
On average, it takes 6 months from the appearance of the first symptoms of sarcoma to diagnosis and initiation of treatment. There were cases when this period was 4-6 years.
Pulmonary sarcomas are primary and secondary. Primary tumors form directly in the lungs. Secondary sarcomas are metastases that have spread to the lungs from tumors that have arisen in other parts of the body.
Depending on the type of tissue from which tumors arise, doctors distinguish the following types of sarcomas:
Myogenic and angiogenic sarcomas are the most common.
The rate at which pulmonary sarcomas metastasize varies greatly depending on the histological type of tumor and individual factors. Most neoplasms of this type are highly aggressive – they quickly penetrate the surrounding tissues and spread to distant areas of the body. Most often, lung sarcomas metastasize to the pleura, brain, liver and adrenal glands.
As mentioned above, lung sarcoma can be primary or secondary. Secondary lesions develop due to the spread of a tumor localized in another part of the body. Sarcomas are quite aggressive tumors. Most often they metastasize to the lungs:
In 19% of patients, the lungs are the only metastatic site. Sarcomas of any subtype have the potential to metastasize to the lungs, but osteosarcomas, synovial tumors, and liposarcoma are most prone to this.
The development of pulmonary metastases negatively affects prognosis: without treatment, most patients die within 6–11 months after diagnosis. Chemotherapy remains the standard approach in the treatment of sarcomas. However, if it is used alone, survival rates improve only slightly. At the same time, surgery can significantly prolong the life of patients.

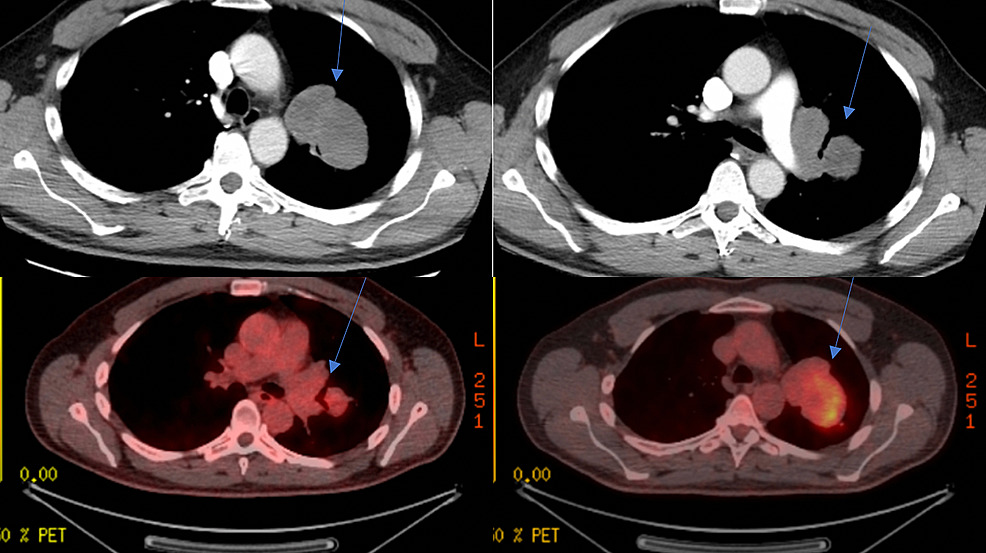
Diagnosing primary pulmonary sarcomas is a rather difficult process, since they are very rare. Lung carcinomas are detected 700 times more often. Symptoms of the disease are nonspecific and the main task of doctors is to distinguish the primary tumor from the metastatic one, since sarcomas of bones and soft tissues often metastasize to the lungs.
One of the main diagnostic methods is x-ray examination. Next, oncologists prescribe a puncture biopsy and histological analysis of sputum. Additionally, CT, MRI and PET-CT may be prescribed to assess the extent of tumor spread.
Since lung sarcoma is a rare disease, its diagnosis and treatment should be carried out by a doctor who has previously encountered it. Leave a request in the form below, and the MedTour coordinating doctor will select for you an oncologist specializing in the treatment of sarcomas.
More recently, scientists have discovered that malignant tumors have molecular differences, even if they are localized in one part of the body. These differences have made it possible to create drugs that specifically target tumor cells. Targeted drug molecules recognize specific mutations on the surface of pathological cells and specifically attack them. Since normal cells do not carry these specific mutations, healthy tissue is not affected by targeted therapy.
To find out whether targeted therapy will be effective in a particular patient, it is necessary to create a molecular portrait of the tumor and find out whether there are target proteins on the surface of its cells. Similar tests are carried out in the best diagnostic centers in the world. Leave a request in the form below, and the MedTour coordinating doctor will select for you a clinic or laboratory that performs molecular genetic research in the field of oncology.
A retrospective analysis of the Surveillance, Epidemiology and End Results database showed that the 5-year survival rate of patients with primary lung sarcoma was:
Thus, surgical treatment allows to achieve the best result. However, this study involved standard radiation therapy. In recent years, lung sarcoma has begun to be treated using stereotactic radiosurgery (CyberKnife technology).

The main reason for poor tumor control with conventional radiation therapy is insufficient total radiation dose. CyberKnife delivers a much higher biologically effective dose compared to standard radiotherapy. In addition to this direct effect of killing tumor cells, CyberKnife destroys the vascular bed of the tumor, causing it to shrink in size.
For early-stage non-small cell lung cancer, stereotactic radiosurgery is the standard option for patients who are medically inoperable or who refuse surgery. For primary lung sarcomas, CyberKnife began to be used relatively recently. But there is already evidence that at an early stage, targeted radiation can destroy the tumor without surgery.
Leave a request in the feedback form below. The MedTour coordinator will select a doctor for you who will be able to determine whether treatment with stereotactic radiosurgery will be effective in your particular case.
In most cases, pulmonary sarcoma can be treated with organ-preserving surgery: lobectomy, economical lung resection. The need for total pneumonectomy is primarily due to damage to the main bronchus or the gigantic size of the tumor. If the malignant process spreads to adjacent structures, an extended or combined pneumonectomy is performed.
Because of their anatomical location around the aortic arch, the left vagus nerve and recurrent laryngeal nerve are frequently affected by hilar malignancies. For the same reason, these nerves may be cut during lung tumor resection or mediastinal lymph node dissection. Nerve damage causes dysfunction of the left vocal cord, which in turn leads to varying degrees of glottis insufficiency and swallowing problems. During resection of lung cancer, vocal cord paralysis occurs in approximately 10% of patients.
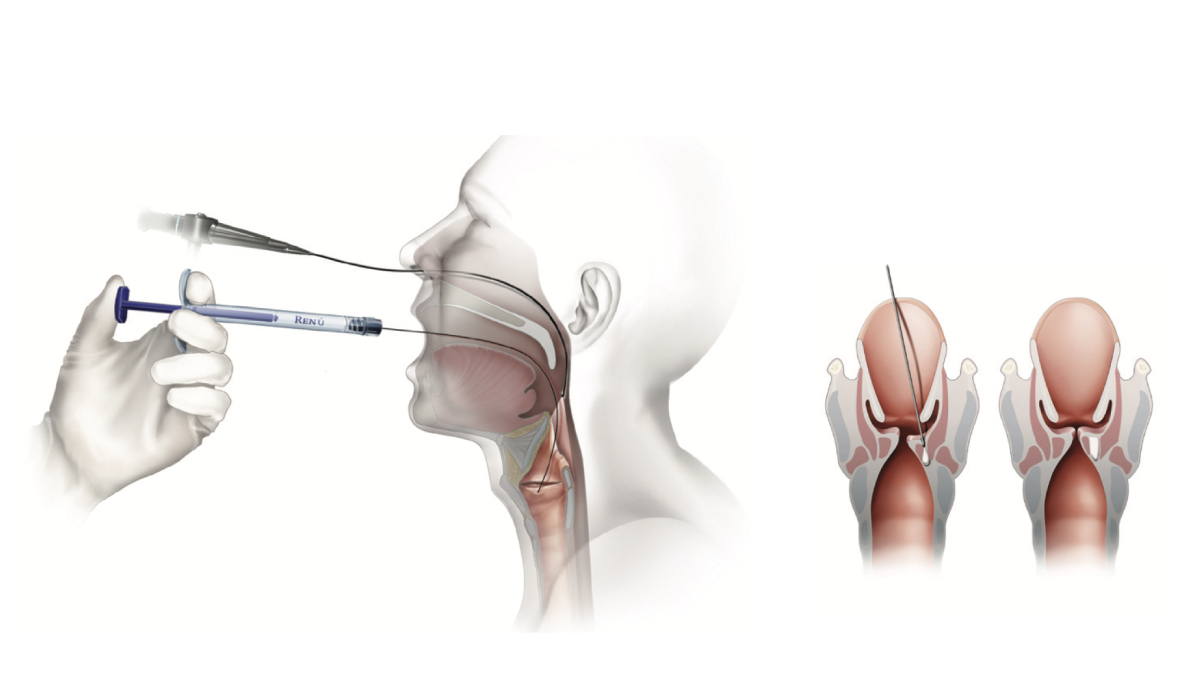
Currently, there are progressive methods for treating laryngeal paresis and restoring voice. Virtus Medical Center has been using injection laryngoplasty and augmentation rhinoplasty since 2015. The SmartCell biotechnological laboratory, which operates at the center, has developed an innovative method for producing a graft from a patient’s adipose tissue. At the same time, platelet-rich plasma is injected into the vocal cords.
The essence of the technique is to augment (build up) a paralyzed ligament in order to restore the normal function of the ligamentous apparatus. The effectiveness of the method is very high. More than 90% of patients report an improvement in their voice after the procedure. Leave a request in the feedback form below to learn more about the innovative method of treating laryngeal paresis.
Primary pulmonary sarcoma is a very aggressive malignancy. It has a significantly worse median 5-year survival rate (35%) than soft tissue sarcomas of the extremities (71%).
In the surgical treatment of patients with pulmonary sarcoma, the size of the primary lesion, histological structure, the condition of the intrathoracic lymph nodes and the degree of tumor differentiation play a role. The best 5-year survival rates can be achieved with:
With myogenic sarcoma of the lungs, the prognosis is unfavorable and amounts to 33.3%.
MedTour company cooperates with the best clinics around the world. Currently, we can offer lung cancer treatment in Turkey, Germany, Spain, Italy, South Korea and other countries where the field of oncology is well developed. Leave a request in the feedback form below to receive a free consultation. The MedTour coordinator will select for you the best oncology center specializing in the treatment of sarcomas, and will also help resolve all organizational issues.
Lung sarcoma is very rarely diagnosed, so it is important to find a doctor who has experience treating this disease. Leave a request in the form below to receive a free consultation. The MedTour coordinator will select an oncologist who specializes in the treatment of lung cancer and sarcoma in particular.
Please rate the work of MedTour
