Calls for Ukraine
Calls for Europe
Calls for USA
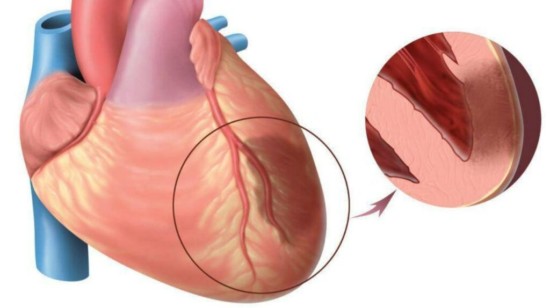
Myocardial infarction (MI), commonly known as a heart attack, is a serious condition that occurs when blood flow to part of the heart muscle is blocked, resulting in damage or death of heart muscle cells.
Here are some statistics related to this phenomenon:
The most common cause of a heart attack is atherosclerosis, which is a buildup of fatty deposits or plaque in the arteries that supply blood to the heart. When one of these plaques ruptures, a blood clot can form that blocks blood flow to the heart muscle.
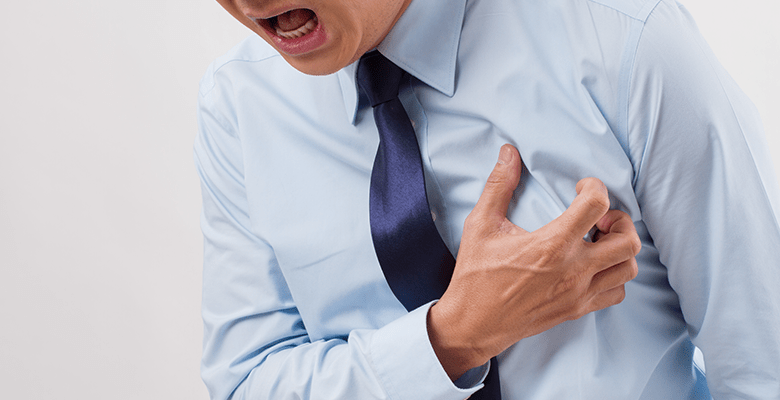
Symptoms of myocardial infarction may include chest pain or discomfort, shortness of breath, sweating, nausea, vomiting, dizziness, and fatigue.
Risk factors for myocardial infarction include smoking, high blood pressure, high cholesterol, obesity, physical inactivity, and a family history of heart disease. Early initiation of treatment is critical to reduce damage in a heart muscle malnutrition condition. Many healthy lifestyle factors such as not smoking, maintaining a healthy weight, regular exercise, and a healthy diet can help reduce the risk of heart attack.
Symptoms of a heart attack can vary from person to person, but most commonly they include:
A condition that can turn into a myocardial infarction is called angina pectoris and manifests itself in much the same way. Small differences in the intensity of symptoms can be noted.
Chest discomfort or pain: this can be like pressure, squeezing, a bursting feeling or pain in the center of the chest. It may last a few minutes or even go away completely. When compared with the pain manifestations of an already occurring myocardial infarction, the pain during a heart attack does not go away and does not become less, sometimes narcotic analgesics are required for relief. Before the onset of an attack, pain may be present for several days or even weeks with varying intensity.
If you suspect you’re having a myocardial infarction (heart attack), it’s important to seek emergency medical attention right away. Call the local emergency number (for example, 111 in Ukraine) or go to the nearest hospital emergency room.
For primary diagnosis, simple methods are used, the equipment for which is available in any medical institution. To clarify the clinical picture and the degree of damage, expensive and invasive methods are used:
Treatment includes a combination of medications, medical procedures, and lifestyle changes. The main methods of treatment:

Myocardial infarction can lead to various complications that complicate the lives
of patients and lead to discomfort. Some of these complications are life-
threatening. These complications can be divided into acute and chronic.
Acute complications include heart failure, thrombosis, cardiogenic shock.
Heart failure is a condition in which the heart cannot pump enough blood to meet the body’s needs. It occurs when the heart muscle is damaged or weakened during a heart attack. It is accompanied by symptoms such as weakness, malnutrition of the brain, shortness of breath and cold. In this case, the functions of all organs suffer. Also often there are arrhythmias — a condition when the heart rhythm is not regular. In this case, the heart may contract too often, but not strong enough, or vice versa — too rarely. Arrhythmia can be either minor and manifested by little
shortness of breath or not at all, or deadly, leading to such a dangerous complication as fibrillation, which is deadly. Since arrhythmia may not occur simultaneously with a heart attack, but later, a patient who has had a myocardial
infarction needs to be under medical supervision for some time. A very formidable complication is cardiogenic shock — this is a serious condition when the heart cannot pump enough blood to the vital organs of the body. This can occur as a result of a severe heart attack and may require emergency treatment such as mechanical circulatory support.
Thrombosis is a very dangerous complication. During a heart attack, the rate of blood flow changes, most often slowing down. In addition, heart attacks are most common in the elderly and in people with atherosclerosis. These factors in combination provide a change in the rheological properties of blood (the properties of blood while it flows through the blood vessels) in the direction of thrombosis.
During a heart attack, most often blood clots form in large vessels, therefore, a frequent complication of myocardial infarction is a formidable complication – pulmonary embolism (PE) — blockage of the pulmonary artery by a thrombus. This complication often leads to the death of the patient. Chronic and delayed complications
Such complications also include arrhythmias, but only if they persist on an ongoing basis. The risks in this case remain the same as in the acute phase. Heart failure in almost all cases of myocardial infarction occurs in the acute phase and persists in one form or another for life. The degree of chronic heart failure is usually much less than in the acute phase, but it is no longer possible to completely get rid of it. There are even less common, but quite significant complications for patients — pericarditis and ventricular aneurysm. Pericarditis: Inflammation of the lining around the heart, known as pericarditis, can occur after a heart attack. This can cause chest pain, fever, and other symptoms. Ventricular aneurysm: A weakened area of the heart muscle may bulge, forming a ventricular aneurysm. Ventricular (less often atrial) aneurysm is usually the cause or additional cause of heart failure or arrhythmia.
Rehabilitation after a myocardial infarction is an important part of the recovery process. The state of health of the patient after a heart attack and the duration of his life depend on the quality of rehabilitation. The rehabilitation program usually includes a personalized exercise program designed to help patients gradually increase their physical activity. This may include aerobic exercise such as walking or cycling, as well as strength training to improve muscle strength. At the same time, patients should receive complete and accessible information about their condition, including information about risk factors, lifestyle changes and medication prescriptions. They can also learn stress
management techniques such as deep breathing and meditation. The rehabilitation program is usually long and includes regular visits to the doctor with adjustments to the rehabilitation plan as needed. Certain drug treatment is both an important part of the rehabilitation process and an element of the subsequent permanent lifestyle. Most patients will need to take medication on an ongoing basis to control their blood pressure, cholesterol levels, and other risk factors for heart disease.
In conclusion, a few words should be said about the prevention of myocardial infarction. There are a few simple steps that can help prevent myocardial infarction:
Troponin levels are elevated during myocardial infarction and may remain elevated for days afterward. Normally, the level of this protein is 0.2 — 0.5 ng / ml, during a heart attack, its level rises 37-400 times.
Medications used in the treatment of this condition may include aspirin, heparin, thrombolytic drugs, beta-blockers, and others.
Patients who survive this clinical situation should follow a diet rich in vegetables,
fruits, fish, whole grains, low in fat, sugar and salt.
Please rate the work of MedTour
