Calls for Ukraine
Calls for Europe
Calls for USA
What is neuritis? This is a pathological condition of the peripheral nerve, characterized by its inflammation. Depending on which nerve is involved in the inflammatory process, doctors distinguish neuritis of:
Simultaneous inflammation of several nerves is called “polyneuritis” or “polyneuropathy.” If only one nerve is affected, it is called “mononeuritis.”

The danger of inflammation of the facial nerve is that, in addition to severe pain, serious complications may develop, for example:
Synkinesis comes in a variety of forms, but they are all united by the inability to perform the desired facial movement in full and the addition of another (involuntary) movement of the facial muscles.

Neuritis (inflammation) of the facial nerve can have a variety of causes, but most often it occurs due to:
Neuritis of the facial nerve can be primary (develops after hypothermia) and secondary (caused by all other reasons).
The pain is acute. It can be compared to an electric shock – sharp, burning, sometimes unbearable. Depending on which branch of the nerve is affected, the pain can radiate to the upper or lower jaw, temples and forehead, manifest as acute “toothache”, and provoke migraines.
Severe and sharp pain can occur in response to touching the face, brushing teeth, facial muscle movements, or shaving. At the same time, an attack differs from a toothache in duration (a toothache usually lasts from 10 minutes to several hours).
At the same time, pain attacks last about 3 minutes on average; there can be up to 200 such attacks per day. According to statistics, in approximately 7% of all patients, pain attacks last up to 3 days.

Inflammation of the facial nerve in children is a fairly common occurrence, especially with the onset of cold weather. Due to the proximity of the nerve to the surface of the skin in children, it is easy to become cold or injured.
The cause of facial neuritis in children may be:
Inflammation of the facial nerve in children begins with an unpleasant stabbing sensation in the back of the head, a feeling of tension, tingling and “shooting” in the area of the eyes, cheekbones and forehead.
After some time, the tingling develops into an attack-like pain, which can be provoked by brushing your teeth and washing your face, sometimes even by a light blow of wind. Often the pain appears in the evening and interferes with night sleep.
Attacks of pain occur from several times a day to several times a week, after which a short remission occurs. Then the pain returns with renewed force, becoming sharp and intense, affecting the area of the eyebrows, eyes, cheekbones, and cheeks.
There is also congenital neuritis of the facial nerve, which is manifested by paresis of the facial muscles. Its cause is improper development of the brain in the prenatal period.
Ignoring symptoms, as well as self-medicating, is very dangerous. Complications from the disease can develop very quickly, especially in children.
The specificity of facial neuritis is that the disease develops abruptly, literally within a few hours. Symptoms of neuritis are divided into early and late.
Early symptoms of neuritis include:
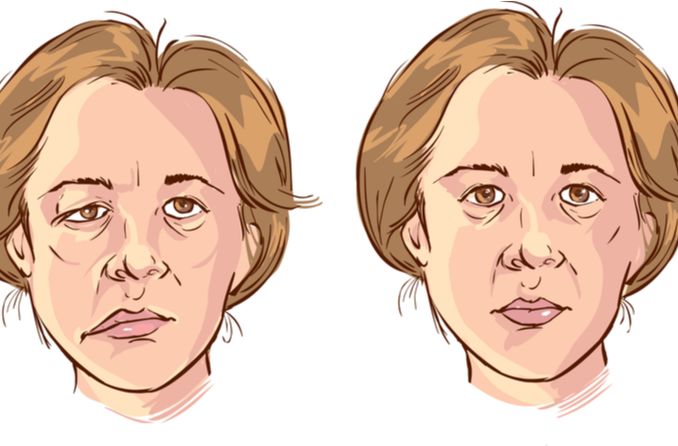
Subsequently, due to severe swelling and pinching of the nerve in the bone canal, numbness and paresis of the facial muscles develop. Paresis differs from paralysis in that muscle mobility is severely limited and does not disappear completely. The following happens:
Depending on the cause, doctors distinguish two types of neuritis of the facial nerve:

To diagnose neuritis of the facial nerve, a doctor first of all conducts an examination, pays attention to how pronounced the asymmetry of the face is, and determines pain in trigger points.
The symptoms of the disease are so vivid that diagnosing neuritis of the facial nerve, based on examination data and the patient’s complaints, is usually not difficult. Doctors pay special attention to how quickly the symptoms grew, how quickly the paresis appeared, whether there were concomitant occurrences, as well as what specifically preceded the onset of the disease and what concomitant injuries or pathologies may be associated with the resulting neuritis.
Additional research methods are also used to diagnose and establish the cause of neuritis:

Treatment is selected individually for each patient after diagnosis and establishment of the type and cause of neuritis. At the beginning of treatment, drug therapy is prescribed, which includes medications and medical procedures aimed at reducing nerve inflammation, relieving swelling and restoring facial movements. Your doctor may also prescribe antibiotics or antiviral drugs if the neuritis is bacterial or caused by a virus.
As paralysis develops, the damaged muscles shorten, which makes it difficult to perform full facial movements. In order to restore facial expressions, physiotherapy is prescribed. Botox injections, in combination with physical therapy, can overcome overstrain of the facial muscles and teach the muscles to move again.
If conservative treatment does not produce positive results, the next step towards recovery is surgery. Surgical treatment for facial neuritis varies depending on the degree of damage to the nerve. The most commonly used types of operations are:
Common practice is to prescribe non-steroidal anti-inflammatory drugs, which have anti-inflammatory and analgesic effects. Painkillers may also be prescribed additionally.
For intense pain and severe nerve damage, doctors may recommend a short course of glucocorticosteroids to relieve inflammation and alleviate symptoms of the disease.
If the cause of neuritis is an infection (bacteria or virus), antibiotics or antivirals are prescribed.
If dry eyes occur, special drops are recommended to moisturize the eyes, or it is possible to cover the eyes with a special bandage at night.
The treatment does not require the patient to stay in the hospital and can be carried out at home, under the supervision of the attending physician.
Facial neuritis is a disease that is treated by a neurologist.
To achieve success in treatment and rehabilitation, you may also need the help of related specialists – a neurologist-rehabilitation specialist, dentist, otolaryngologist, traumatologist, ophthalmologist, and for children, a consultation with a pediatrician is also required.
There are a number of measures that will help prevent inflammation of the facial nerve. These include:

For rehabilitation, physiotherapeutic procedures, laser, heating and massages are used, aimed at restoring the nerve and motor activity of facial muscles.
While 3 weeks (sometimes up to several months) are often enough to overcome pain, restoring facial expressions after paresis or paralysis is a more complex process that takes a longer time. However, if you contact specialized rehabilitation clinics that use the best equipment and have qualified doctors, the rehabilitation process will go faster. In this case, there is a much greater chance of complete restoration of facial movements and facial symmetry.
The prognosis depends on many factors, such as the cause of inflammation, which part of the nerve is damaged, and whether there are complications.
If symptoms gradually subside during the first three weeks after treatment, this is a good sign. In this case, you can expect a complete recovery. In 75% of all cases, complete recovery occurs.
If the disease lasts longer than 3 months, the chances of full recovery of facial expressions are somewhat reduced.
With relapses of facial nerve neuritis, each subsequent episode of exacerbation will be more difficult.
MedTour employees have many years of experience helping patients with a wide variety of diseases and conditions. Our medical coordinator will help you choose the best clinic for diagnosis and treatment of neuritis in Ukraine or abroad.
The MedTour company cooperates with leading clinics in Ukraine and abroad, having the opportunity to quickly contact them and determine the most comfortable conditions for treating patients.
Please rate the work of MedTour
