-
 News
When glucose levels are low, chemotherapy ceases to affect cancer cells
News
When glucose levels are low, chemotherapy ceases to affect cancer cells
-
 News
Excessive treatment of prostate cancer in older men may reduce quality of life without increasing its duration
News
Excessive treatment of prostate cancer in older men may reduce quality of life without increasing its duration
-
 News
Brain cancer can be cured by viruses
News
Brain cancer can be cured by viruses
-
 News
Ways to reduce lymphatic pain in breast cancer have been found
News
Ways to reduce lymphatic pain in breast cancer have been found
-
 News
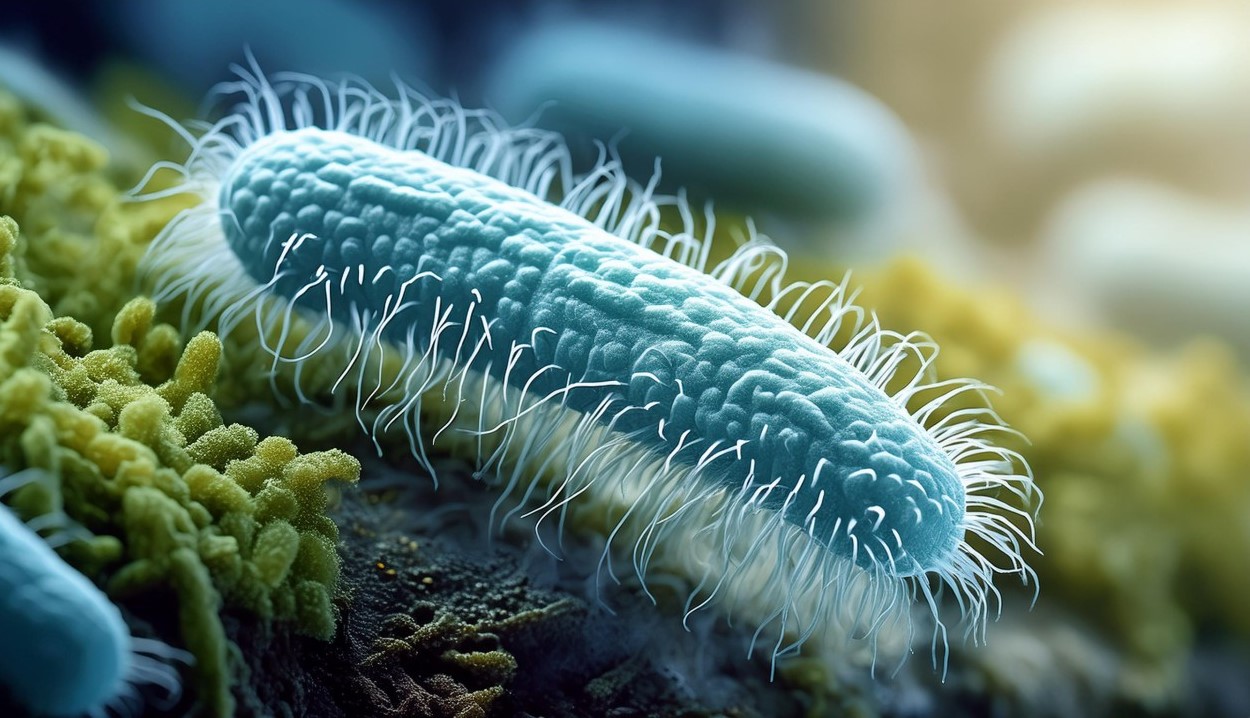
Scientists have turned bacteria into a powerful weapon against cancer
News
Scientists have turned bacteria into a powerful weapon against cancer
All news
Spinal cord tumors treatment
Spinal cord tumors are pathological growths that are located in the spine or spinal cord. These tumors cause pain, neurological problems, and sometimes paralysis. A spinal tumor is life-threatening and can cause permanent disability.
According to the WHO, spinal cord tumors account for 2-4% of all tumors of the nervous system and occur with a frequency of 10 cases per 100,000 people.
Diagnostics: MRI, X-ray, CT, PET, myelography.
Treatment: conservative therapy, microsurgery, radiation and chemotherapy.
MedTour patients recommend clinics for the treatment of spinal cord tumors:
Doctors for the treatment of spinal cord tumors
Patient reviews
Frequently Asked Questions
Spinal cord tumors, or spinal tumors — neoplasms that grow from a mutated cell that has begun to divide uncontrollably in the spinal cord.
- Much less often brain tumors develop;
- Most often they are formed at the age of 30-50.
By origin, spinal tumors are distinguished:
- Primary (benign or malignant) — occur directly in the spine and spinal cord;
- Secondary (exclusively malignant) — metastases of another cancer that have reached the spine.
Spinal tumors are also divided into types depending on their location to the spinal cord and its hard shell:
- Extradural — outside hard shell of spinal cord;
- Intradural — in a hard shell. There are such types:
- Intramedullary — inside the spinal cord;
- Extramedullary — outside the spinal cord. Such neoplasms are divided into:
- Subdural — under the hard shell;
- Epidural — above the hard shell.
The reasons for the development of primary spinal neoplasms are unknown.
In most patients, these tumors are spontaneous, i.e. appear without any provoking factors. A small percentage of patients have a hereditary disease that promotes the development of tumors.
Lifestyle and dietary habits, stress, smoking or excessive alcohol consumption don’t play a role in the development of primary spinal cord tumors.
The most common representatives of various types of spinal tumors:
- Known extradural neoplasms — lymphomas, sarcomas, osteomas, chondromas;
- Frequent intramedullary tumors — ependymomas, astrocytomas, hemangioblastomas;
- Common extramedullary tumors — meningiomas, schwannomas, ependymomas.
Neoplasms differ from each other in their growth rate, their relation to neighboring tissues and their ability to metastasize.
- Malignant tumors grow rapidly and penetrate into adjacent tissues. In addition, it can metastasize, that is, spread cancer cells throughout the body through the blood or lymph;
- Benign tumor doesn’t have the properties listed above. On the contrary, such a tumor grows slowly and doesn’t grow into adjacent tissues. In addition, it does not metastasize and cannot recur.
In general, the manifestations are diverse, depending on the neoplasm site. Typical symptoms:
- Pain;
- Numbness;
- Weakness in the arms and legs;
- Erectile dysfunction;
- Incontinence of urine or feces.
Many neoplasms are benign. With timely complete removal of the tumor, the chances of recovery are good.
- Timely treatment of extramedullary tumors often leads to recovery.
- The prognosis for intramedullary tumors is less favorable, since the risk of disability is higher.
With secondary neoplasms, the prognosis is more favorable with early diagnosis and timely treatment.
Modern methods of diagnosis and treatment of spinal cord tumors
Spinal cord tumor diagnostics
The first step towards detecting spine neoplasms is a consultation with narrowly specialized specialists — a neurologist and a spinal surgeon.
Doctors will prescribe a range of laboratory tests: blood and urine tests. Sometimes a cerebrospinal fluid test may be required.
The most important test — an MRI (magnetic resonance imaging) scan with or without contrast. Foreign clinics are equipped with high-power MRI, which have high resolution and information content. These characteristics allow experienced physicians to detect compression of the spinal cord and its roots.
MRI of the spinal cord — the method of choice that visualizes the smallest structures and reveals the slightest deviations from the norm.
Other diagnostic methods:
- X-ray;
- CT (computed tomography) with myelography. With this method, the doctor finds out the location of the tumor;
- PET (positron emission tomography).
Spinal tumors compress the spinal cord, causing dysfunction and irreversible degenerative changes. Therefore, it’s important to diagnose the tumor as early as possible and start therapy immediately. Prompt treatment helps prevent permanent damage.
Spinal cord tumor treatment
If the manifestations indicate that the tumor is pressing on the spinal cord, experienced doctors immediately prescribe high doses of corticosteroids to reduce the swelling.
If the neoplasm cannot be removed, radiation therapy (RT) is used. Sometimes RT is used after surgery to relieve pressure on the spinal cord.
Chemotherapy may be used depending on the type of cancer.
Spinal surgery:
The only radical treatment for a significant portion of spinal tumors is their surgical removal.
The goal of the surgery — to unload the nerve structures by removing the tumor and stabilizing the destroyed parts of the vertebra with metal implants. Thus, pain, neurological symptoms and emotional disorders of the patient are reduced and eliminated.
Removal of a benign tumor leads to a complete cure. In case of malignant neoplasms, RT and / or chemotherapy are performed after surgery.
For intramedullary tumors, surgical tactics and / or radiation therapy are used.
Extramedullary or extradural tumors are treated with additional chemotherapy as needed.
Qualified foreign surgeons prefer spinal surgery according to the following criteria:
- The risk of wound infection is lower;
- Less blood loss during surgery;
- The restoration of body structures is faster;
- The number of drugs used during the operation is less;
- Doctors make minimal incisions, avoiding large tissue incisions;
- Rehabilitation is faster and the hospital stay is reduced to 2-3 days.
Published:
Updated:










Велика подяка за життя. Возняк Олександр Михайлович, Зенкевич Ярослав Павлович.
Кажуть Феофанія для міністрів, ні ця лікарня для людей. І я цьому приклад. Кожного року після операції присилаю МРТ на контроль. Ні разу не відмовили. Всіх пам’ятають, хоч я простий український роботяга. Ці люди від Бога, для людей!